Written by
Zoë

Reviewed by
Henry Dornier
Published on
Jan 15, 2026
One compliance slip can cost your agency its carrier contracts. Medicare agent training is how you protect your business while building a team that performs.
What is Medicare agent training?
Medicare agent training is the ongoing process of coaching agents after they're licensed. It covers product knowledge, sales skills, and compliance with CMS regulations.
Licensing proves that an agent met the minimum requirements. Training is what turns that baseline into real performance. Plans change, rules update, and beneficiaries expect agents who know their stuff.
This training happens through call reviews, coaching sessions, role-playing, and real-time feedback. The goal is to build agents who can guide beneficiaries to the right plan while staying compliant on every call.
Why Medicare agent training matters
Medicare sales is one of the most regulated spaces in insurance. CMS sets strict rules for how agents can market, communicate, and enroll beneficiaries. Breaking those rules has real consequences.
The stakes are high and getting higher
An estimated 73 million baby boomers will reach Medicare age by 2030. That's a massive wave of beneficiaries who need guidance. More volume means more calls, more opportunities, and more chances for compliance mistakes. Agencies that can't train agents fast enough will struggle to keep up.
Compliance violations are expensive
CMS can issue fines, suspend agents, or terminate their ability to sell Medicare products. Carriers can drop agencies that rack up complaints. One bad call can trigger an audit that puts your entire book of business at risk. The financial and reputational damage can take years to recover from.
AEP creates intense pressure
The Annual Enrollment Period (AEP) runs from October 15 to December 7. That's less than two months to handle new enrollments and renewals.
Agents work at high volume under tight deadlines, which makes training gaps even more dangerous. There's no time to fix mistakes when every day counts.
Beneficiaries are protected consumers
Medicare beneficiaries are often seniors making complex healthcare decisions. Many are going through the system for the first time.
CMS rules exist to protect them from misleading sales tactics. Agents who don't understand these rules can harm vulnerable people and expose your agency to liability.
Turnover makes training essential
Insurance sales have high turnover. New agents join, experienced agents leave, and product details change every year.
Without consistent training, knowledge gaps grow, and compliance risks multiply. Agencies end up in a constant cycle of onboarding without ever building real expertise.
Overview: What Medicare agent training covers
Training area | What it covers | Why it matters |
|---|---|---|
Product knowledge | Plan types (Medicare Advantage, Supplements, Part D), network restrictions, annual changes, and plan comparisons | Agents who don't know the products can't guide beneficiaries to the right choice |
CMS compliance rules | Scope of Appointment: | Violations lead to fines, suspensions, or losing the ability to sell Medicare |
Sales conversation skills | Opening calls, uncovering needs, presenting options, handling objections, knowing when to recommend | Compliance and sales work together; poor conversations lead to complaints |
Documentation and recording | What to document, Scope of Appointment forms, Call recording disclosures | Records protect the agent and agency if a complaint arises |
Key areas to cover in Medicare agent training
Good Medicare agent training goes beyond product knowledge. Agents need to know how to help beneficiaries, follow CMS rules, and keep the agency out of trouble.
Product knowledge
Agents need to understand the plans they sell. This includes Medicare Advantage, Medicare Supplements, and Part D prescription drug plans.
Training should cover:
How each plan type works
Network restrictions and out-of-pocket costs
Annual changes during the AEP and the Open Enrollment Period (OEP)
How to compare plans based on beneficiary needs
Agents who don't know the products can't guide beneficiaries to the right choice. That leads to complaints, disenrollments, and compliance flags.
CMS compliance rules
CMS has specific rules for Medicare sales. Agents must follow these rules on every call and at every appointment.
Key compliance areas include:
Scope of Appointment: Agents can only discuss plan types that the beneficiary agreed to in advance. Bringing up other products without permission is a violation.
No cold calling: Agents cannot make unsolicited calls to sell Medicare products. The beneficiary must request contact first.
Enrollment periods: Agents can only enroll beneficiaries during valid enrollment windows (AEP, OEP, SEP). Enrolling someone outside these periods is a violation.
Required disclosures: Agents must identify themselves, state they're selling insurance, and provide specific disclaimers.
No misleading statements: Agents cannot misrepresent plan benefits, costs, or coverage.
Training should include real examples of violations and how to avoid them. Agents need to know what they can and cannot say.
Sales conversation skills
Sales and compliance go hand in hand. Agents have to ask good questions, listen to beneficiaries, and present plans clearly. Doing one well means doing the other well.
Key areas to focus on:
How to open a call and set expectations
Questions to uncover beneficiary needs (doctors, medications, budget)
How to present plan options without being pushy
Handling objections while staying compliant
When to recommend a plan vs. when to let the beneficiary decide
Role-playing is effective here. Agents can practice conversations and get feedback before talking to real beneficiaries.
Documentation and recording
CMS requires agents to document enrollment conversations. Many agencies also record calls for quality assurance and compliance.
Training should cover:
What to document and when
How to complete the Scope of Appointment forms
Call recording requirements and disclosures
How documentation protects the agent and the agency
Agents who skip documentation steps create risk. If a complaint arises, the agency needs records to defend itself.
Common challenges in Medicare agent training
Training Medicare agents is not easy. Agencies face several challenges that make consistent coaching difficult, such as:
Managers can't review every call
A busy agency might have dozens of agents making hundreds of calls per day. Managers can only listen to a small sample. Compliance issues slip through because no one catches them. By the time a problem surfaces, it may have happened on dozens of calls.
Training is inconsistent
Different managers coach differently. One might focus on sales technique while another focuses on compliance. Agents get mixed messages about what matters. Without a standard approach, quality varies from team to team.
New agents struggle without support
New agents often handle calls alone before they're ready. They make mistakes, get frustrated, and leave. High turnover creates a cycle where agencies are always training but never building expertise. The cost of recruiting and onboarding adds up fast.
Compliance rules change
CMS updates its marketing guidelines regularly. Carrier rules can change too. Keeping agents current on every rule is a constant challenge, especially when updates drop right before AEP.
Remote teams are harder to coach
Many Medicare sales teams work remotely. Managers can't walk the floor and listen in. Coaching happens through scheduled calls, which limits how much feedback agents receive. Issues that would get caught in an office go unnoticed for weeks.
How AI coaching improves Medicare agent training
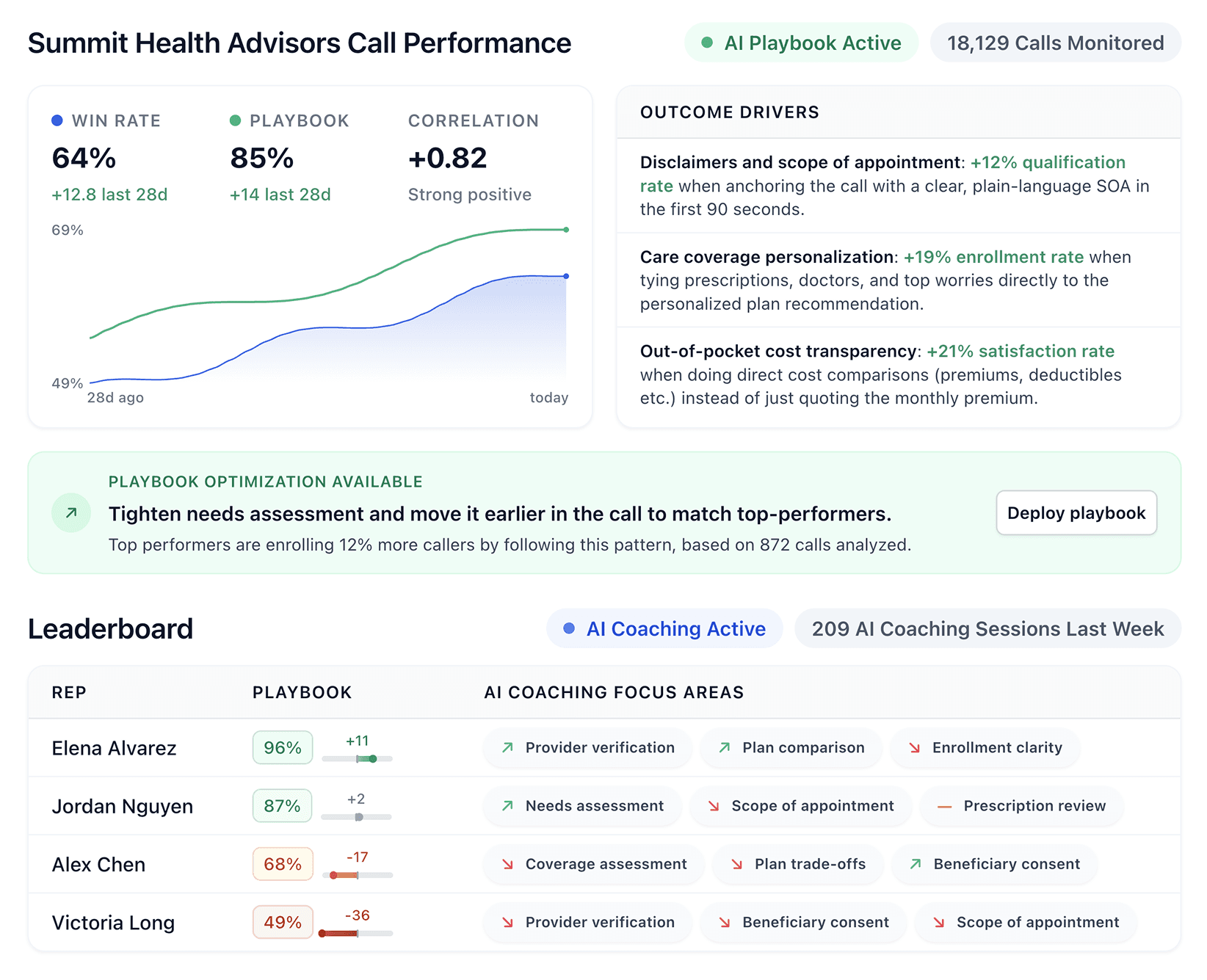
AI coaching tools solve the challenges above. They monitor every call, guide agents in real time, and scale feedback across your whole team.
Playbook-driven coaching trained on your rules
What happens if CMS audits 10 calls from last month? Would your team pass? Generic coaching tools can't help you answer that. They tell you when agents talk too much or miss an objection. They don't catch a skipped disclosure or an SOA violation.
Playbook-driven AI does. It learns your compliance rules, your required disclosures, and your approved scripts and language.
For example, you can:
Add simple criteria like a recording disclosure that agents must read on every call.
Include complex criteria such as your SOA verification process.
Build checks that confirm agents followed CMS enrollment rules.
Track how many enrollments met compliance requirements.
It catches the mistakes that generic tools miss because it's trained on your specific rules, not generic best practices.
Real-time guidance to prevent violations
New agents face a tough choice: Wait until they're fully trained and miss AEP, or take live calls before they're ready and risk violations. Real-time guidance removes that tradeoff. New agents can take live calls while getting prompts that keep them compliant.
The benefits of this new approach are that they:
Build confidence with a safety net.
Gain experience without putting the agency at risk.
Get training on the job, in real time.
Compliance tracking at scale
One missed disclosure is a coaching moment. You pull the agent aside, remind them of the rule, and move on. But patterns tell a bigger story:
Twenty missed disclosures from the same agent signal a performance issue.
Five agents making the same mistake signals a training gap.
AI spots these patterns across thousands of calls and shows you where problems are forming. You fix root causes instead of chasing one incident at a time.
Targeted coaching for each agent
Managers can't listen to every call and write feedback for every agent. There's not enough time. AI picks up the slack by reviewing calls and creating coaching notes for each agent.
Each note includes:
What happened on the call
What went wrong
How to fix it
Managers review them, add their thoughts, and send. Agents get real feedback without managers spending hours on call reviews.
AI voice agents for after-hours lead handling
Cold callbacks don't work like warm conversations. When an agent calls a lead back 12 hours later, the beneficiary has to remember who you are and why they reached out. The momentum is gone.
AI voice agents keep the lead engaged overnight because they:
Have a real conversation with the beneficiary
Qualify their needs
Schedule a specific follow-up time
The next morning, your agent picks up a warm conversation instead of making a cold callback.
HIPAA and SOC 2 Type 2 compliant
Beneficiaries trust you with sensitive information. They share details about their health, their medications, and their finances. A platform that doesn't protect that data puts that trust at risk.
If a breach happens and their information gets exposed, the relationship is over. HIPAA and SOC 2 Type 2 compliance show you take their privacy seriously.
Building a Medicare agent training program
Here's how to structure a training program that keeps agents compliant and performing:
Start with compliance fundamentals
New agents need compliance training before they take their first call. Teach them CMS rules, carrier guidelines, and your agency's own policies. Then test them. You want to know they actually understand the rules and can apply them on a live call.
Create a playbook for your team
Document your sales process step by step. Include required disclosures, approved language, and examples of compliant conversations.
This playbook becomes the foundation for all coaching and sets the standard for every agent. When questions come up, agents have a single source of truth to reference.
Use call reviews for ongoing training
Review calls regularly for both compliance and sales techniques. Share examples of good calls so agents know what to aim for, and calls that need improvement so they learn from real mistakes.
Make feedback specific and actionable. Vague advice like "be more compliant" doesn't help anyone improve.
Provide real-time support
New agents make mistakes in the moment, so they need help in the moment. Real-time coaching tools give them prompts while they're on the call. A small slip gets corrected before it turns into a compliance violation on a recorded line.
Track metrics that matter
Compliance flags deserve as much attention as conversion rates. Track how many calls include required disclosures. Measure how often agents go off-script. Use this data to identify training needs and catch patterns before they turn into bigger problems.
Update training as rules change
CMS updates guidelines before each AEP, and carriers may change their rules too. Build a process for updating your playbook and retraining agents on new requirements. An outdated playbook creates compliance risk even for agents who follow it perfectly.
Make Medicare agent training work with Alpharun
Medicare agent training is essential for compliance and performance, but scaling it is hard. Managers can't review every call, and generic coaching doesn't address CMS-specific rules.
Alpharun helps Medicare sales teams train agents more effectively:
Build custom playbooks from your best calls so that every agent learns what compliance looks like in practice.
Coach agents in real-time with prompts that prevent CMS violations before they happen.
Track compliance across every call so nothing slips through.
Send targeted coaching notes based on each agent's specific gaps.
Handle after-hours leads with AI voice agents that stay compliant and keep prospects warm.
Protect beneficiary data with HIPAA and SOC 2 Type 2 security.
Medicare agent training protects your agency and your beneficiaries. Alpharun makes it easier to deliver that training at scale.
Book a demo to see how Alpharun helps Medicare agencies train more agents with less risk.