Written by
Eloisa Mae

Reviewed by
Paul Dornier
Published on
Jan 28, 2026
Your Medicare floor has a handful of reps who hit quota and a majority who don't. The gap isn't talent. It's talk track. The right Medicare sales strategies turn what your top performers actually say into a repeatable, compliant playbook for everyone else.
Why Medicare sales strategies matter now
Over 34 million people are now enrolled in Medicare Advantage, which is 54% of those who qualify. The market's gotten crowded, compliance rules are stricter, and clients are facing an average of 32 plan options. Most don't know where to begin.
Agents who rely on generic pitches struggle to stand out. Meanwhile, top performers follow proven systems that build trust quickly and guide clients toward confident decisions.
13 Medicare sales strategies for high-volume call centers
Each strategy breaks down into three parts: a rep move with exact language, a manager move that shows how to coach it, and a QA item that keeps the behavior consistent across the floor.
1. Lock down permission to contact before any pitch
Outreach rules shape your whole funnel. Medicare.gov says plans can't call unless the person is a member or has given permission to contact. Skip this step, and every call that follows sits on a compliance violation.
Most reps treat permission as a throwaway line at the start of the call. Top performers treat it as a gate. They confirm permission, log it, and only then move forward.
This small discipline protects the rep, the manager, and the organization from complaints that snowball during audits.
Rep example: "Do I have your OK to call you about Medicare plan options you asked about?"
Manager coaching note: Train one sentence for permission and one sentence for next steps. This is a compliance checkpoint, not a rapport moment. Don't let reps improvise or bury it in small talk.
QA item: Permission captured and logged before plan discussion.
2. Use a 60-second needs check that feeds plan fit
High-volume calls need a repeatable path to fit. When reps ask different questions in different orders, managers can't compare calls or coach patterns. The result is a floor full of reps running their own versions of discovery, with no way to identify what works.
A standardized needs check solves this. Three questions, same order, every call:
Doctors first: Network fit is often the deal-breaker.
Medications second: Drug coverage drives cost.
Benefits third: Extras like dental or vision tip the decision when plans look similar.
When every rep follows the same structure, you can see which talk tracks convert and which stall. Manual QA can't do this at scale. You need AI that analyzes patterns across thousands of calls.
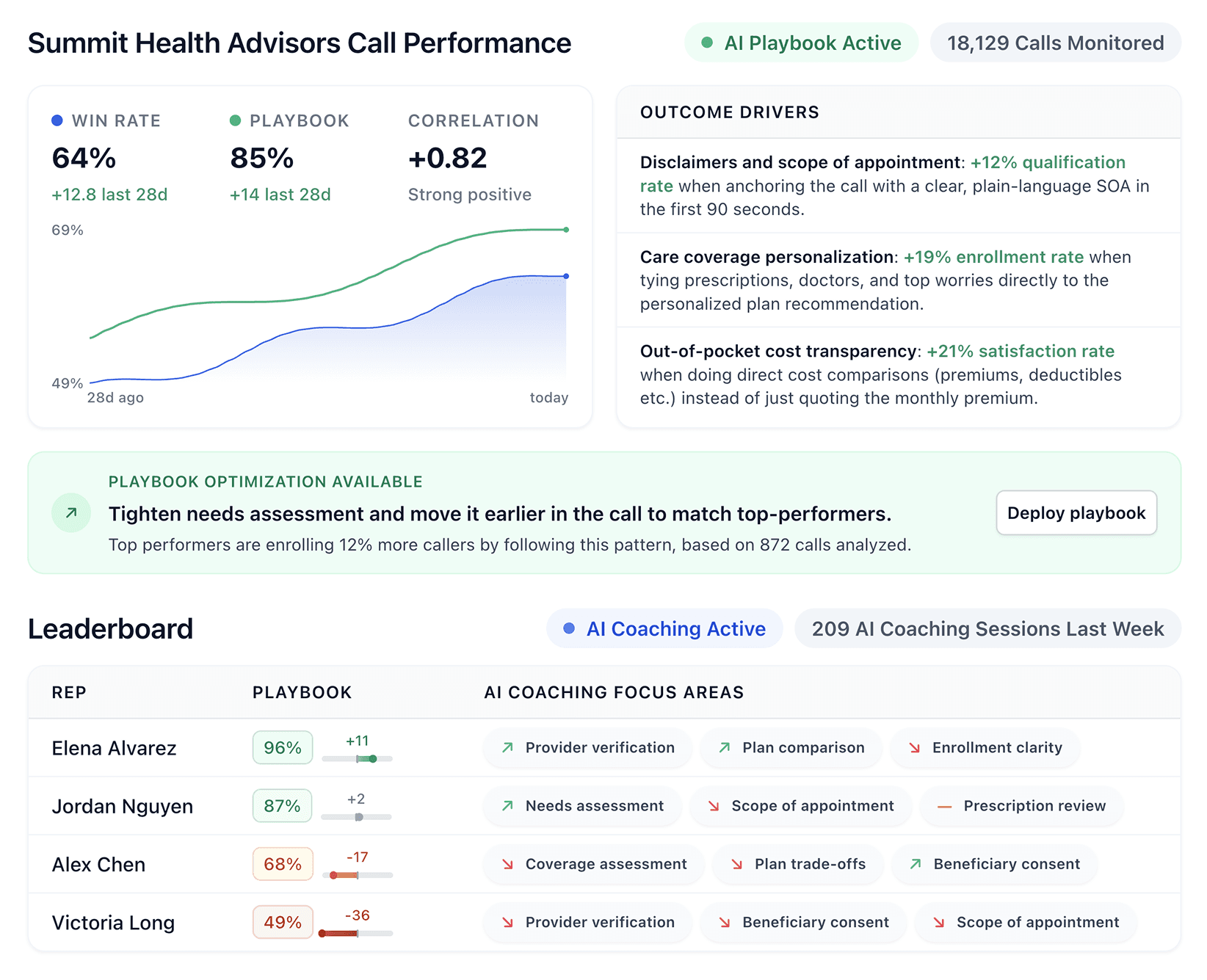
That's what Alpharun does. It makes this visible by analyzing thousands of calls to surface patterns that managers would never catch manually.
Rep example: "What doctors do you want to keep? What meds do you take? What benefits matter most?"
Manager coaching note: Build a script that asks the same three questions on every call. Order matters.
QA item: Needs questions asked before any plan comparison.
3. Turn "active listening" into a labeled recap
Generic listening advice tells reps to "reflect back what they heard." That's vague, and vague advice produces inconsistent behavior. A labeled recap gives reps a concrete move: summarize the prospect's needs in one sentence, then ask for confirmation.
This does two things:
First, it reduces backtracking. When the prospect confirms the summary, both sides know they're aligned before costs come up.
Second, it cuts hold time. Reps who recap before quoting don't have to circle back when they realize they missed something.
Rep example: "You want to keep Dr. Martin, you take two generics, and dental matters. Did I get that right?"
Manager coaching note: Coach reps to recap before quoting costs. The recap confirms understanding and gives the prospect a chance to correct errors before the conversation moves forward.
QA item: Rep confirms needs summary with a yes from the prospect.
4. Explain costs with two buckets and a third guardrail
Prospects get lost in Medicare terms. Maximum Out-of-Pocket (MOOP), copays, coinsurance, deductibles, and networks. When reps explain each term separately, prospects tune out or get overwhelmed. A bucket frame organizes the information so prospects can compare plans without drowning in jargon.
Bucket one is the worst-case cost: the maximum they'd pay in a bad health year.
Bucket two is everyday cost: the copays they'll see at the doctor or pharmacy.
The guardrail is network fit: whether the plan covers their doctors and pharmacies. This frame lets prospects ask better questions and make faster decisions.
Rep example: "Bucket one is the worst-case medical cost. Bucket two is your day-to-day copays. Guardrail is your doctor and pharmacy network."
Manager coaching note: Require reps to say the guardrail line every time. Network fit is where most plan switches fall apart. Make sure reps address it before the prospect asks.
QA item: Rep covers MOOP, copays, and network check.
5. Compare plan types without steering
Medicare rules warn against steering and pressure language in meetings. Reps who push one plan type over another create compliance risk and erode trust. The prospect feels sold to instead of helped, and the call center faces audit exposure.
Top performers present options neutrally and let the prospect choose a direction. "Option A is this, Option B is that. Which do you want to explore first?"
This approach respects the prospect's autonomy and keeps the rep on the right side of compliance. Once the prospect picks a direction, the rep can go deep without triggering pressure flags.
Rep example: "Option A is Original Medicare plus a supplement. Option B is a Medicare Advantage plan. Which option do you want to explore first?"
Manager coaching note: Train "choice first" language before details. Let the prospect pick a direction, then go deep on that option.
QA item: No "best plan" claims or pressure lines.
6. Use a "screen-share style" talk track on voice calls
Transparency builds trust even when reps can't share their screen. When reps describe what they're checking, prospects feel included instead of waiting in silence.
This matters because Medicare prospects are making a high-stakes decision about their health coverage, and silence feels like uncertainty.
Narrating the verification process slows the call slightly but reduces callbacks from prospects who felt rushed or confused. Both sides stay aligned, and the prospect hears that their information is being handled carefully.
Rep example: "I'm checking three items now. Your zip code, your doctors, and your prescriptions."
Manager coaching note: Require reps to name the checks out loud. The small time investment pays off in fewer callbacks and higher close rates.
QA item: Rep describes the verification steps before making a recommendation.
7. Build an AEP calendar that protects manager coaching time
AEP volume spikes and coaching stops unless it's scheduled. Managers who coach reactively end up firefighting instead of improving rep performance.
Protecting coaching time means treating it like any other meeting. Block 30 minutes per day, keep the block fixed, and don't let call volume push it out. Short daily sessions compound over the enrollment period.
Rep example: "I can book your review now. Morning or afternoon works better?"
Manager coaching note: Set daily coaching blocks and keep them fixed. Even 30 minutes per day compounds over the enrollment period.
QA item: Appointment offered and booked when the call intent fits.
8. Use the Scope of Appointment controls for scheduled meetings
CMS requires a documented Scope of Appointment for marketing activities. The SOA must list product types and the appointment date. Missing this step creates audit exposure that compounds across hundreds of calls.
The fix is simple: Add an SOA checkbox to the dialer workflow. Make it impossible for reps to skip. When reps capture the SOA before the meeting content begins, they're protected and the call center has documentation if questions arise later.
Rep example: "This appointment covers Medicare Advantage and Part D. You can add other topics later if you want."
Manager coaching note: Add an SOA checkbox to the dialer workflow. Make it impossible for reps to skip this step.
QA item: SOA captured before the meeting content begins.
9. Keep educational events clean, then convert after
Medicare.gov says plans can't market or enroll people during educational events. Mixing education and sales in the same session creates compliance violations. The event becomes a sales pitch disguised as education, and attendees feel misled.
Separate event scripts from sales scripts. Educational events explain Medicare concepts without recommending specific plans, and reps who want to follow up do so in a separate conversation after the event ends. This keeps the event clean and creates a natural handoff to sales.
Rep example: "Today is Medicare 101 only. People who want plan help can request a follow-up."
Manager coaching note: Separate event scripts from sales scripts. Different talk tracks, different goals, different compliance rules.
QA item: No plan enrollment or plan push during education events.
10. Treat D-SNP calls as eligibility first, benefits second
Dual-Eligible Special Needs Plan (D-SNP) eligibility depends on Medicaid status and level, so reps who lead with benefits waste time on unqualified prospects. The call drags on, the prospect gets excited about benefits they can't access, and both sides leave frustrated.
Confirming Medicaid status in the first 60 seconds keeps the call focused. Qualified prospects move into a benefits conversation with confidence. Unqualified prospects get redirected to other options before anyone wastes time.
Rep example: "Do you have Medicaid today? Do you have a card that shows your level?"
Manager coaching note: Build a short eligibility decision tree. Reps should know within 60 seconds whether a D-SNP conversation makes sense.
QA item: Rep verifies eligibility signals before discussing D-SNP benefits.
11. Replace referrals with "pass my card" language
Medicare's one-on-one meeting guidance says agents may leave business cards but may not ask for names and numbers to sell to friends or family. The line between a referral and a violation is thin.
"Pass my card" language stays compliant. The rep offers their contact info for the prospect to share, but never asks for third-party details.
Rep example: "If a friend needs help, you can share my number. You never need to give me their info."
Manager coaching note: Ban any request for contact lists. Train reps on exactly what they can and can't say about referrals.
QA item: No request for third-party names or numbers.
12. Build a banned-phrases library tied to compliance scoring
Medicare.gov lists examples of pressure and misleading behavior to avoid. A banned-phrases library makes this concrete: instead of vague guidance like "don't pressure prospects," reps see exact phrases to avoid and approved alternatives.
The library works best when it's tied to compliance scoring. Tools like Alpharun automatically flag calls with banned phrases, so managers review them before complaints escalate and risk drops across the floor over time.
Rep example:
Avoid: "You have to join, or you won't have coverage."
Use: "You can choose to change plans during Open Enrollment if you want."
Manager coaching note: Review one banned phrase per day in team huddles. Short, repeated exposure builds awareness faster than long training sessions.
QA item: Auto-flag calls with pressure phrases for manager review.
13. Make QA a coaching loop instead of a scorecard
QA works when it drives behavior change. A scorecard that grades reps without coaching them creates anxiety but doesn't improve performance.
A coaching loop connects scores to specific improvements. When a rep gets flagged for skipping the needs check, the manager coaches that behavior in the next session. One behavior per rep per week, based on trend data.
This is where tools like Alpharun change the math. Instead of spot-checking a handful of calls, Alpharun scores 100% of calls automatically and sends reps coaching notes tied to specific moments. Managers see trends, reps get actionable feedback, and scores improve.
Rep example: "Let me recap what you told me, then we'll compare options."
Manager coaching note: Coach one behavior per rep per week, based on trend data.
QA item: One coaching action logged per flagged theme.
What makes Medicare call centers hard to scale
Scaling a Medicare call center means getting consistent results from dozens or hundreds of reps. These three problems make that harder than it looks:
1. Managers coach from a tiny sample of calls
When you're listening to five or ten calls per rep each week, you're guessing at patterns. You might catch a blown objection or a compliance slip, but the gap between what "good" sounds like and what reps actually say stays invisible. Coaching becomes reactive instead of strategic.
2. Compliance rules raise the stakes on every conversation
Medicare places strict limits on outreach, gifts, and what agents can discuss in meetings. One wrong phrase can trigger a complaint, and complaints compound fast in high-volume environments.
When reps learn bad habits early, you're not losing deals. You're building risk into every call they make.
3. AEP pressure floods the floor with volume
The Medicare Annual Enrollment Period (AEP) runs from October 15 to December 7, and call counts spike faster than most teams can absorb. Coaching time disappears right when reps need it most. The same reps who struggled before AEP now have even less support during the year's highest-stakes window.
Medicare sales strategy: What's working vs. what's not
Before adding new tactics, check whether your current playbook transfers from top performers to everyone else.
Area | Warning signs | Signs it's working |
Performance gap | Your top 10% closes at double or triple the rate of everyone else, and nobody can explain why. Tribal knowledge runs the floor. | The middle 60% starts sounding like the top 10%. Close rate rises while complaint rate stays flat. |
Playbook clarity | Managers coach with phrases like "build rapport" and "overcome objections." Reps nod along in training, then freeze on live calls. | New reps know what to say in the first 30 seconds. The playbook includes exact phrases, not just concepts. |
QA coverage | You're spot-checking five calls a week, hoping to catch the problems. Risk phrases spread because patterns go unnoticed. | Every call gets scored against clear standards. Managers coach trends instead of hunting for examples. |
A rep who closes deals but triggers complaints isn't a winner worth copying. Look at the close rate and the compliant close rate together.
How to scale winners across every rep with Alpharun
Medicare call centers run thousands of short calls per day during AEP. Managers can't listen to all of them, and spot-checking misses the patterns that matter.
Alpharun closes that gap:
Custom playbooks: Built from your actual calls, capturing the exact behaviors that drive Medicare conversions.
AI coaching: Sentence-level feedback during and after calls so reps improve faster.
Manager visibility: Dashboards showing where reps follow or miss the playbook, including compliance steps.
100% call scoring: Every call is graded against your standards, not just the handful that managers can review.
Alpharun is SOC 2 Type 2 compliant and integrates with Five9, Genesys, and other major platforms. Most teams go live in about a week, which means you can onboard before AEP and see results during enrollment season.
The playbook that works for your best reps becomes the standard. AI agents handle the calls that don't need human judgment.
Schedule a demo to see how Alpharun turns your top performers' Medicare sales strategies into the floor-wide playbook.