Written by
Zoë

Reviewed by
Paul Dornier
Published on
Jan 14, 2026
Healthcare call centers cost $13.9 million per year to run, and 39% of leaders cite agent burnout as their biggest source of waste. These 17 healthcare call center best practices help high-volume sales teams protect that investment.
Essential healthcare call center best practices
These practices cover everything from HIPAA compliance and AI coaching to agent training and playbook development. Here's how top-performing teams put them to work:
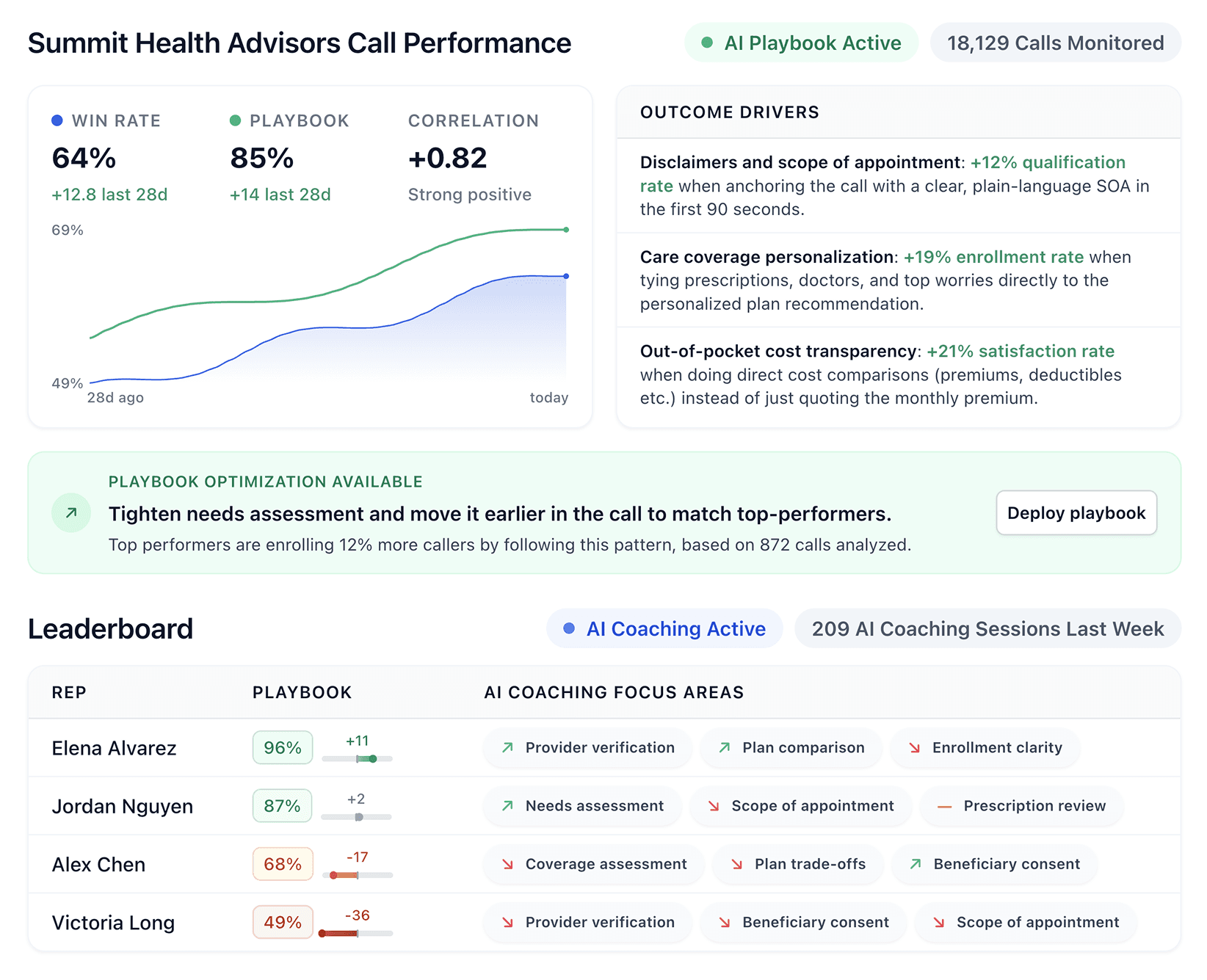
1. Build playbooks from your actual winning calls
Generic scripts from the internet won't help your team close more deals. One of the most important healthcare call center best practices is studying your own top performers to find out exactly what works.
Look for patterns in how your best reps:
Handle objections when a Medicare beneficiary pushes back on price
Ask discovery questions in a specific order
Use phrases that move hesitant callers toward enrollment
Close using language that resonates with your customer base
Document these patterns into a custom playbook. New hires learn what actually works in your business instead of theory from a textbook.
2. Score 100% of calls (not random samples)
Managers typically review 5-10 calls per rep per week. When reps handle 30, 40, or 50 calls daily, most conversations never get feedback.
AI-powered scoring tools analyze every call against your playbook criteria. You see exactly where reps follow the process and where they drift.
Patterns emerge across hundreds of conversations, showing you which skills need work across the whole team and which reps need individual attention.
3. Make compliance part of the scoring model
In healthcare sales, compliance isn't separate from performance. They're the same thing.
Your scoring should include:
Recording disclosure read on every call
Required Medicare/insurance disclaimers delivered correctly
Verification protocols followed before discussing Protected Health Information (PHI)
Proper documentation of scope of appointment
When compliance criteria live inside your coaching system, reps don't see it as an obstacle. It becomes part of how they succeed.
Build checks for your qualification process too. Monitor how many sales closed AND how many met all compliance rules. A sale that triggers a compliance violation isn't a win.
4. Give reps real-time guidance during calls
Post-call feedback helps, but real-time coaching transforms performance.
When a rep hits a tough objection mid-call, they need help NOW. The best coaching tools provide instant prompts based on what's happening in the conversation.
A caller mentions they're on a fixed income, and a prompt appears: "Here's how your top performers handle this..." The rep adjusts their approach and keeps the call moving forward.
This levels the playing field between experienced reps and new hires. Everyone gets access to the collective wisdom of your best people, exactly when they need it.
5. Send coaching notes directly to reps
Managers don't have time to deliver personalized feedback to every rep after every call.
Automate this. After each call, reps should receive short, digestible notes highlighting what they did well and what to improve. Keep it specific: "At 2:34, you missed an opportunity to ask about their current coverage. Try this question next time..."
This takes work off the manager's plate. Reps get continuous improvement without waiting for their next 1:1.
6. Encrypt everything (calls, texts, chats)
The Health Insurance Portability and Accountability Act (HIPAA) requires protecting patient health information across all channels. That means encrypting every call recording, text message, chat conversation, and voicemail.
The cost of getting this wrong is massive. Fines reach $71,162 per violation, annual caps can exceed $2 million for repeated breaches, and one Anthem data breach resulted in a $16 million penalty.
Before signing any contract, verify your vendors have SOC 2 Type II certification and HIPAA compliance. Use platforms that encrypt data in transit and at rest, and always ask for proof.
7. Control access to patient information
Not everyone on your team needs access to all patient information. Limit access based on what each role actually requires, and build systems that track who touches what.
Your access control checklist should include:
Role-based permissions so reps only see data required for their job
Logging every access attempt for audit purposes
Regular log reviews to catch unusual patterns
Immediate access revocation when employees leave the company
Documentation retention for six years (some states require longer)
Former employees with lingering system access cause preventable breaches. A simple offboarding process stops this problem before it starts.
8. Train on HIPAA annually (at minimum)
A covered entity must train all workforce members on policies and procedures appropriate to their functions. One-time onboarding training isn't enough because rules change, people forget, and new threats emerge.
Annual refresher training keeps HIPAA top of mind. Include real scenarios your reps face, like what to do if a caller asks you to send information to a family member, or how to verify identity before discussing coverage details.
Document every training session with records of who attended and what you covered. You'll need this when auditors come knocking.
9. Use AI voice agents for after-hours and repetitive tasks
About 11% of patient calls come in after-hours or on weekends. Most go to voicemail and never get a callback. That's lost revenue.
AI voice agents capture these leads instead. They handle:
After-hours lead qualification
Appointment scheduling and confirmations
Initial information gathering
Routine follow-up calls
Your human reps should spend time on conversations that need expertise and empathy. Let AI handle the repetitive work that doesn't require human judgment. This gives you 24/7 coverage without hiring night shift staff.
10. Reduce hold times below 60 seconds
The average hold time in U.S. healthcare call centers is 4.4 minutes. The industry target is 50 seconds.
Long hold times kill conversions. About 16% of callers hang up before reaching an agent. Every abandoned call is potential revenue walking out the door.
Solutions that work:
Better call routing to match callers with available reps
Callback options so callers don't wait on hold
AI agents handling simple inquiries to free up human reps
Accurate staffing models based on call volume patterns
Track Average Speed to Answer (ASA) weekly. If you're consistently above 60 seconds, something needs to change.
11. Track metrics that predict revenue
Generic metrics like average handle Time don't tell you if reps are closing deals. Track what actually predicts revenue instead:
Metric | Why it matters |
|---|---|
Playbook adherence | Shows whether reps follow the talk tracks that win deals |
Conversion rate by stage | Reveals where deals fall apart in your funnel |
First Call Resolution | Builds trust and reduces costly callbacks |
Compliance score | Tracks how many calls meet regulatory requirements |
Ramp time | Measures how fast new hires reach full productivity |
These metrics show you exactly where to focus coaching efforts.
12. Cut ramp time with structured onboarding
Healthcare sales reps take 12-18 months to reach full productivity, compared to 6-9 months in other industries. During this extended ramp period, you may operate at a net loss on that hire.
Speed this up with:
Immediate access to recorded calls from top performers
Real-time coaching during their first live calls
Clear milestones with specific skills to demonstrate
Frequent check-ins during the first 90 days
AI coaching tools help new reps perform better from day one. They get instant guidance instead of waiting months for their manager to notice gaps.
13. Create escalation protocols for urgent situations
Healthcare call centers occasionally receive calls from people in distress. Your team needs clear rules for these moments.
Build your escalation protocol around these elements:
Define exactly when calls escalate to supervisors or clinical staff.
Train reps to recognize language that signals emergencies.
Document every urgent situation for follow-up.
Route high-stress calls to experienced agents who stay calm under pressure.
Identify which reps handle crisis situations well and lean on them.
Not every rep handles high-stress calls the same way, and that's okay. Know who does it best.
14. Collect feedback after every call
Post-call surveys reveal whether your approach builds trust. Keep them short with one or two questions maximum. "Did the agent answer your questions?" and "How likely are you to recommend us?" give you actionable data without annoying callers.
Track satisfaction trends over time. When scores drop, investigate immediately. One bad month can signal a training gap, a new competitor, or a product issue.
15. Fight agent burnout before it starts
Staff burnout and turnover rank as the top sources of inefficiency in call centers. About 39% of organizations cite this as their biggest challenge.
Burned out reps deliver worse customer experiences. They make more compliance mistakes. They quit, forcing you to restart the expensive hiring and training cycle.
Prevention tactics:
Automate tedious post-call documentation.
Provide real-time support so reps don't feel alone on tough calls.
Recognize wins publicly.
Keep caseloads manageable during peak periods.
Invest in technology that makes the job easier, not harder.
16. Update your playbook continuously
What worked last quarter may not work next quarter because Medicare rules change, competitor offerings shift, and customer expectations evolve.
Build systems that capture new insights as they happen:
Add new tactics to the playbook as soon as top performers discover them.
Review call data monthly for emerging patterns.
Remove outdated guidance that no longer applies.
Your playbook should be a living document, not a static PDF that gathers dust.
17. Hire for empathy (then train everything else)
You can teach product knowledge, compliance rules, and sales techniques. Empathy is harder to train.
Healthcare callers are often stressed, confused, or scared. They're facing Medicare decisions for the first time, processing a new diagnosis, or worried about costs.
Reps who genuinely care about helping people build trust faster, close more deals, and generate more referrals than those who just want to hit quota.
Screen for empathy during interviews. Use role-play scenarios with emotional complexity and watch how candidates respond when the caller gets frustrated.
Scale your healthcare call center with Alpharun
Several of these healthcare call center best practices require technology that most platforms don't provide.
Most coaching tools weren't built for healthcare. They don't understand Medicare objections, insurance compliance, or what it takes to close a hesitant beneficiary. Alpharun does.
Here's how Alpharun helps healthcare sales teams put these best practices to work:
Custom playbooks from your calls that capture what your top Medicare and insurance performers say when beneficiaries push back or hesitate to enroll.
Compliance is built into every score with automatic checks for disclosures, disclaimers, and verification protocols on every call.
Real-time coaching for tough moments that prompts reps mid-call based on your playbook so they handle objections like your best people do.
AI voice agents for repetitive work that handle after-hours lead qualification and routine scheduling so human reps focus on closing.
Enterprise-grade security with HIPAA and SOC 2 Type II compliance to keep patient data protected across every channel.
Healthcare sales teams need coaching built for regulated industries. Book a demo and see how Alpharun delivers both performance and compliance.